Current Newsletter: Issue One 2023
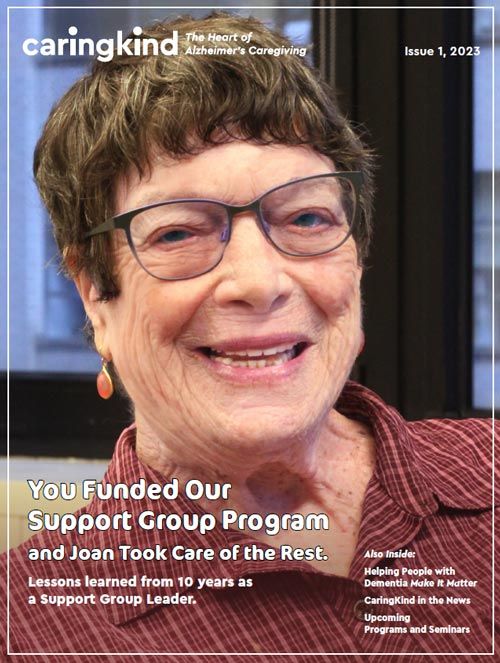
What resonates for me most, as a Support Group Leader, is the interaction between the members of the group. I find it fascinating. They play off each other and it’s like watching a ball bounce around the room. It’s emotional and joyful. And it’s engrossing to watch the group’s involvement with one another.
Read Online Download
Sleep Manual
A Virtual Manual for Nine Ways to Better Sleep
If you are thirty years old, you have been sleeping for about ten years. At age fifty, more than fifteen years. By seventy-five, you’ve racked up a quarter century of sleep. And more than 200,000 hours. How much do you remember about what happened to you as you slept all those years? And how much did you control the time you were asleep? Maybe more than you think you could. You’ve made a good start by enlisting in 9 Ways to Better Sleep. There are several ways to use this manual and participate in the other parts of the program.Learn More Download
Homecare & Nursing Home Booklets
Introducing the CaringKind Comics!

CaringKind's comic that tells the story of one family’s experience with Alzheimer’s disease.
Family Caregiver Guides
The Family Caregiver Guide (FCG) is based on the curriculum for the 10-hour Family Caregiver Workshop offered at CaringKind. The four sections of the FCG correspond with the four sessions of the workshop: Understanding Dementia, Effective Communication, Behaviors Have Meaning, and Caring for the Caregiver.
Finding Comfort: Living with Advanced Dementia in Residential Care
This booklet is for family members, friends and caregivers of a person who has dementia. The purpose is to provide information about the best ways to offer comfort and the best possible quality of life for someone whose dementia is progressing.
Palliative Care for People with Dementia Guidelines
In the absence of a medical cure or effective treatment, families and professional caregivers often feel helpless and hopeless. The principles behind our palliative care project offer help and the promise that we can make a residents’ life better, in some cases with the simple additions of a moment of pleasure; a smile, a hug, a needed nap, a taste of chocolate, or a favorite song.
Read more/Download PDF
ADvancing Care

ADvancing Care is a newsletter for people who work in nursing homes and other residential care settings, and for the families and friends of those who live there.
Read more/Download PDF
Support Group Brochure

Our support groups, led by trained facilitators, provide caregivers with the opportunity to discuss the many challenges of caring for a family member with Alzheimer’s disease and related dementias, with others who understand. Our goal is to provide a safe setting which promotes mutual support, both practical and emotional, throughout the course of the disease.
Read more Download PDF
Archived Newsletters
2022 Volume Four
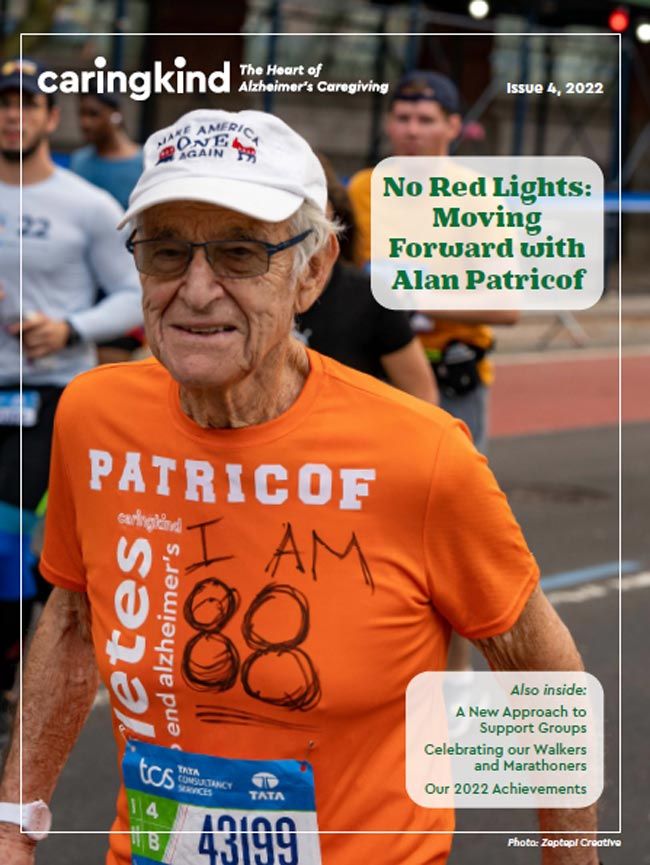
Read online
Download PDF
2022 Volume Three
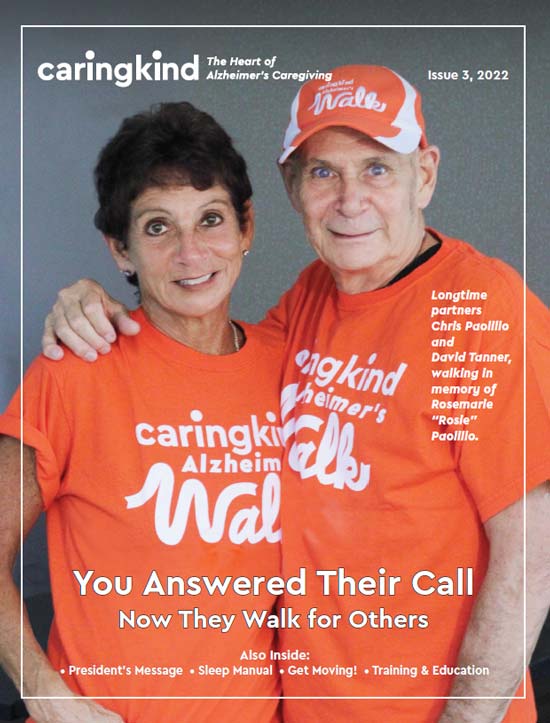
Read online
Download PDF
2022 Volume One
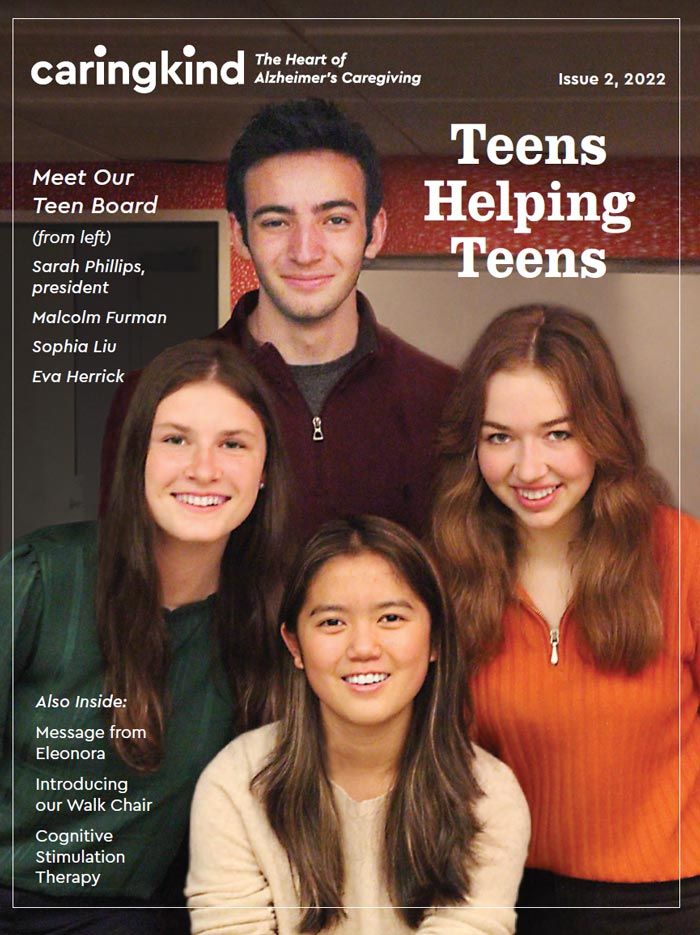
Read online
Download PDF
2022 Volume One
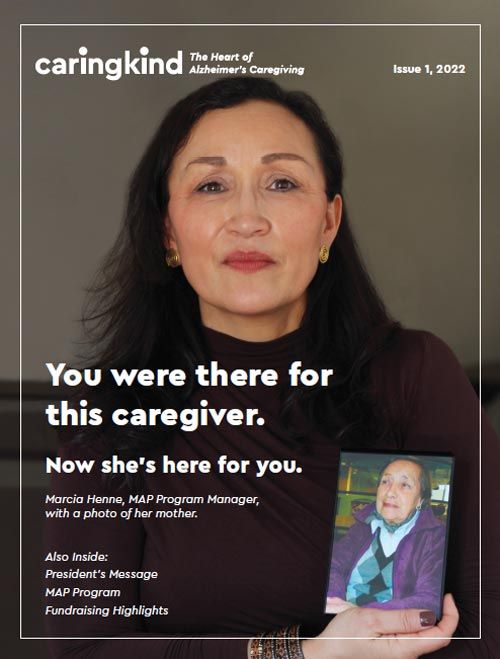
Read online
Download PDF
2021 Volume Four
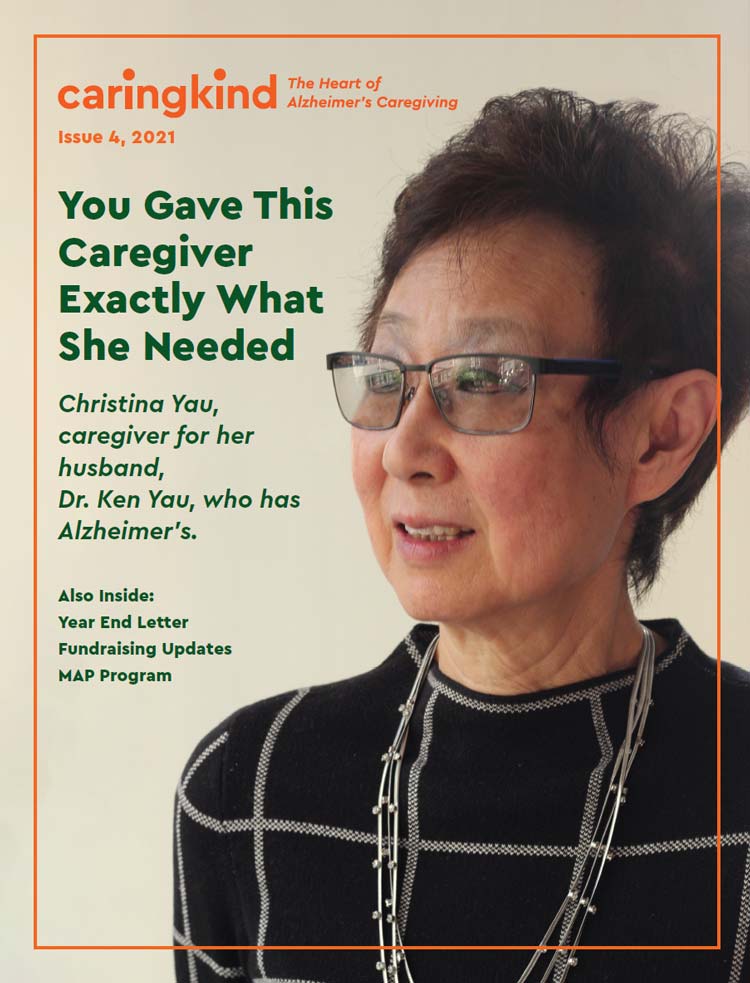
Read online
Download PDF
2021 Volume Three
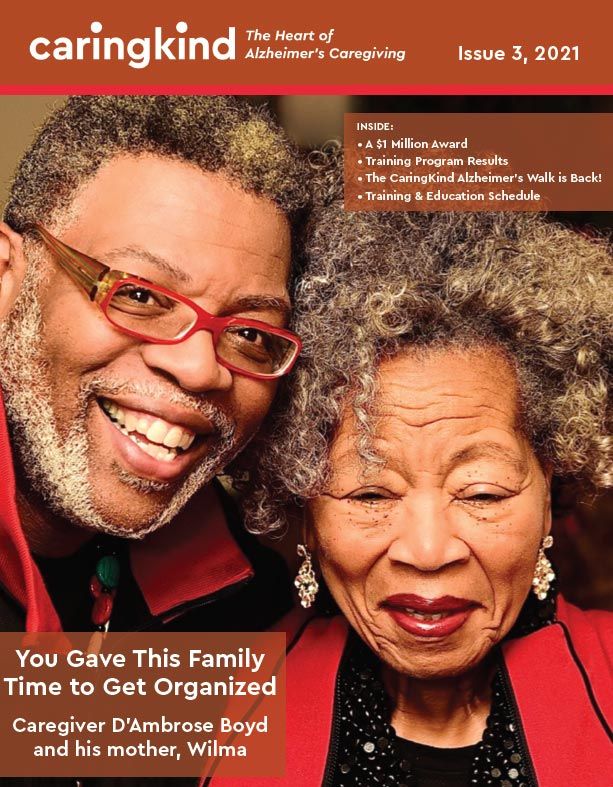
Read online
Download PDF
2021 Volume Two
Read online
Download PDF
2021 Volume One
Read online
Download PDF
2020 Volume Tnree
Read online
Download PDF
2020 Volume Two
Read online
Download PDF
Winter 2019-2020
Read online
Download PDF
Winter 2019-2020
Read online
Download PDF
Summer 2019
Read online
Download PDF
Spring 2019
Read online
Download PDF
Winter 2019
Read online
Download PDF
Fall 2018
Read online
Download PDF
Summer 2018
Read online
Download PDF
Spring 2018
Read online
Download PDF
Winter 2017-2018
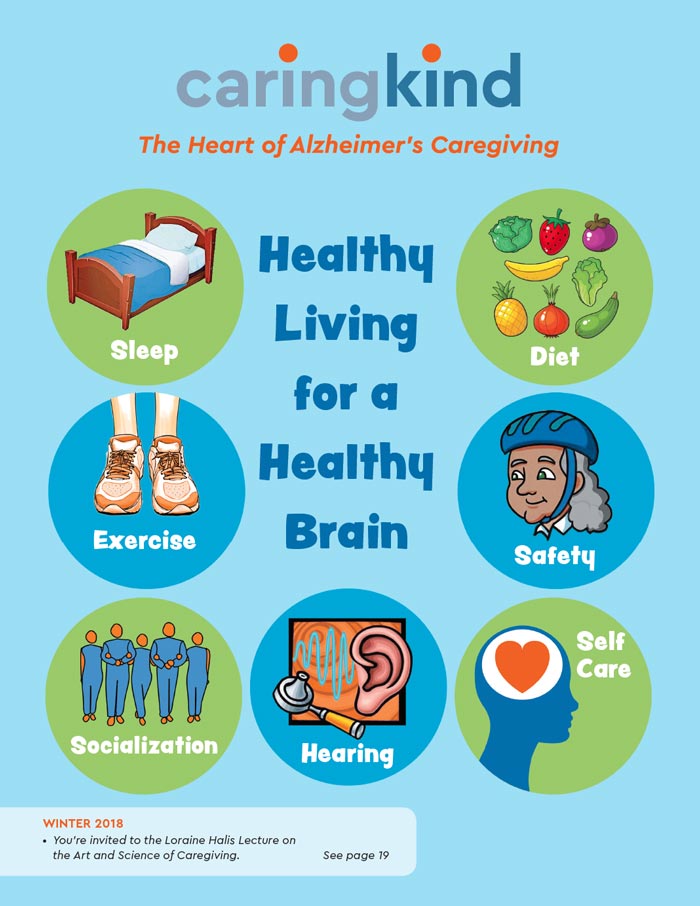
Read online
Download PDF
Fall 2017
Read online
Download PDF
En Español (PDF)
Summer 2017
Read online
Download PDF
Spring 2017
Read online
Download PDF
En Español (PDF)
Winter 2017
Read online
Download PDF
En Español (PDF)
Fall 2016
Read online
Download PDF
En Español (PDF)
Summer 2016
Read online
Download PDF
En Español (PDF)
Spring 2016
Read online
Download PDF
En Español (PDF)